
You can’t really see it here, but #8 is gone.
My son is now fourteen years old, almost fifteen, and in ninth grade. Back in fourth grade, his class was doing a “square dance.” My son fell down, face-down on the floor. Another kid fell on top of his head, smashing his teeth into the floor. He was in braces at the time, and his two central incisors were significantly intruded. He was rushed to the pediatric dentist, who happened to be across the street from his school. She repositioned the teeth and the orthodontist (next door) fixated them using the brackets still attached. I was upset, and my wife wondered why. I knew what was to come.
Endodontic treatment was later done on one of the central incisors. Not long after that, we noticed external root resorption occurring in the cervical region. My endodontist conferred with a respected professor where he did his residency. The conclusion was that nothing could be done about the resorption, and that we’d likely lose the teeth at some point. I hoped we’d have some time… a lot of time.
Over time, it was also apparent that the teeth had ankylosed. As the rest of him grew, the central incisors did not go with the rest of the crowd. For cosmetic reasons, I did some bonding to lengthen the centrals.

Ankylosed centrals resulted in a reverse smile line. Corrected with composite bonding. This was 2 years ago.
Time.. ticking away with my sanity, hard to believe such a calamity
Time’s up! We got almost five years. My son came to me late Saturday night, “I was biting into a cheese stick and my tooth broke.” The entire crown of tooth #8 (the one that was RCT’ed) was mobile and still attached at the gingiva. I broke into a cold sweat. I knew it was coming, and it still REALLY bothered me. I knew this would not be an easy case. My beautiful son, with beautiful teeth… losing his FRONT teeth. And, most of you know that replacing them is no easy task. He’s too young for implants. And, doing a conventional bridge is rather invasive to the adjacent teeth. Flippers just suck. People have said, “He’s lucky his dad is a dentist.” I don’t feel so lucky. I know too much.
I got him into the office today (Easter Sunday), and my wonderful assistant met us there.
We got some x-rays. It was not good. And, I see resorption advancing with #9, too. Shit.
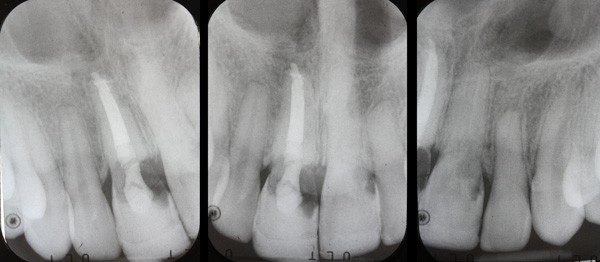
Pre-op x-rays.
They didn’t teach us this in dental school!
I honestly had no idea what I was going to do. I made it up as I went along.
My first thought was to extract the coronal portion of the tooth, fill in the defects and bond it as a “pontic” to the adjacent teeth as an ersatz “Maryland Bridge.” Later I’d have my periodontist extract the root and place a bone graft.

Pre-op. #9 is extruded and “waving in the breeze.”
I anesthetized the area and placed an Optragate for better visualization and access. In the process of inserting the Optragate, the tooth fell out.

Optragate in place. If you’re not using these, you’ve GOT to try them! Makes access and retraction so easy!
Sunday, bloody Sunday…
In the area of resorption, there was a big blob of hyperplastic, red, bleeding tissue which was obscuring the remaining root from view. I used a combination of a Picasso Lite diode laser and currette to clean up the hyperplastic tissue.
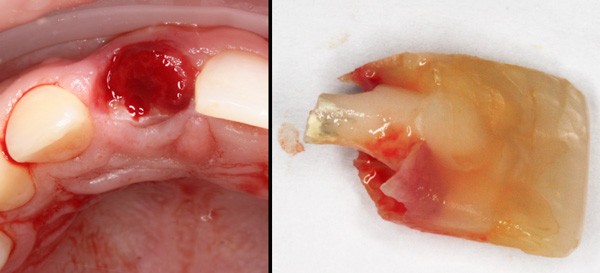
On the right, you can see the composite core placed in the endo access years previously.
Once I rinsed off the exfoliated dental crown and the residual root, I noticed that the resorbed areas were quite clean. It is nothing like decay. It looked like “Pac-man” ate away the dentin, leaving it clean and HARD. It’s not soft like decay, and it’s not discolored.
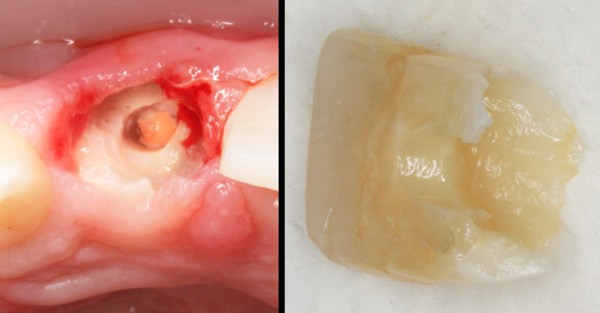
Hyperplastic tissue removed on left. At this point, I had removed (from the crown) the old composite that had filled the endo access.
Paging Dr. MacGyver… Again.
Then I had an idea. What if I placed a post in the remaining root and bonded the crown to that? Hmmmm… How would I fill in the missing areas with composite without having a bunch of excess being expressed into the tissues, not being able to trim the excess and polish it? Wait a sec… I have another idea.
Pressure… pushing down on teeth, pushing down on tooth
I had a model of my son’s teeth from about a year ago in the lab (from making a sports guard). I used my Mini-Star pressure former (Great Lakes Orthodontics) to create a Copyplast matrix (clear and more rigid than bleach material). I’d use this to position the crown properly in the arch.

Pressure-formed Copyplast matrix.
I fitted a 3M Rely-X Fiber Post 3D into the canal and placed it WITHOUT bonding it. I then etched and bonded the tooth and placed it in the Copyplast matrix. Then I put a dab of Filtek Supreme Ultra in the crown, with the idea of picking up the post. I seated the matrix intraorally and visually confirmed that the composite came in contact with the post. Then I used my Ultradent Valo curing light to polymerize the composite through the matrix. I removed the matrix and then the crown of the tooth. Voila! The post came out attached to the crown as planned.
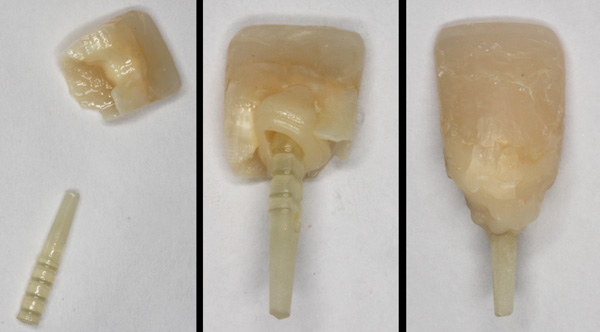
Used crown to pick up post from root.
Next, I got some hot water in a bowl to heat up some Filtek composite. I applied warmed and soft composite to the crown / post and re-seated it in the remaining root, allowing the surrounding tissues to shape the composite. I removed the “restoration” and cured the composite. “Rinse and repeat” with additional increments of composite to fill in the blanks. Then I trimmed and polished the “composite root” structure I had created. I re-seated it in the root to confirm fit.
The idea was to fill in the blanks and trim and polish, as much as I could (extraorally) BEFORE bonding it to the root. I didn’t want a bunch of uncontrolled composite extruding into the supporting tissues.
Don’t drill me. I’m only the hockey player.
My son was getting fidgety and impatient by now. He asked me if we could just leave the tooth out. He didn’t mind the missing tooth… He’s a hockey player. And, he was quite serious. “Sorry, dude… I care, and your mother cares.”

Hockey player smile – Level: Novice!
Next, I applied Surpass (Apex Dental Materials) as a bonding agent to the remaining root and my cobbled restoration. Surpass is a self-etching material that I have found won’t initiate bleeding in delicate exposed soft tissues. I decided to use Geristore glass dual-cure resin-ionomer (Den-Mat) for the “cement,” as it is reportedly well-tolerated by soft tissues when used to restore root lesions / defects. I filled the canal with Geristore and seated the “restoration.” I quickly cleaned up the expressed excess material using a microbrush. Then I zapped it with the curing light. I let it auto-cure the rest of the way for 4 minutes, as stipulated by the instructions for Geristore. Whaaat? A dentist read the instructions??

Immediate post-op.
“Is it in, yet?”
My son had been in the chair for nearly 3 hours. I gave #8 a good tug with my fingers and it appeared to be solid. In the end, the crown was not perfectly aligned. It appeared to be facially-tipped and slightly long. I used a combination of diamonds and polishing instruments to bring it into “alignment.” I then checked and adjusted occlusion so that it wasn’t touching in centric or excursions.
I realize this is temporary at best. It may be VERY temporary. I’m just trying to buy some more time to decide what is next. Do we do a flipper? He’ll hate it and probably won’t wear it. Do we do a traditional fixed bridge, invasiveness be damned? Or what about a zirconia-based Maryland bridge? I’ve done one before. Will the laterals (alone) support a bridge (of either kind)? They don’t look so hot, either. Even when he’s old enough for implants, they are generally contraindicated for hockey players until they “retire.”
I’ll be sharing this with my esteemed colleagues and entertaining any ideas or input. Feel free to chime in with your own in the comments below!
 Copyright protected by Digiprove © 2016-2018 The Dental Warrior®
Copyright protected by Digiprove © 2016-2018 The Dental Warrior® 
Nice job, Dad! Working on family members is not easy, and this one was a doozy!!
That’s a tough case Mike. Especially when it’s your son. Great job on the temporization. Hopefully you can preserve enough bone to place a couple of implants when he’s 18-20. Until then, it will be a balancing act between preserving enough bone and keeping your son smiling. No more cheese sticks! 🙂
Hi Mike,
Tough situation. Unless there is a crowded bicuspid at the right stage to transplant I’d strong recommend extracting ankylosed centrals and moving laterals that direction with orthodontics. If they are ankylosed then damn. Did a case like this a while ago…would need to hunt for the photos. Anyway- if moving, then Maryland to replace the vacant laterals, building up to make them into centrals and place implants in lateral position later (smaller spot with better bone). On that note there is the new idea of grinding up the extracted teeth and using as a graft. Super-cool story.
Flippers do suck, but if it’s unavoidable he will live. I had one from age 9-25, and I turned out ok (mostly;)
Mike, what your son has/had is called Invasive Cervical Resorption. I have had 3 patients in my practice with it. If you look at the radiograph of #9, you can see on the distal the tell-tell signs: Looks like decay, but not really like decay (translucent but has some opacity to it), can’t really see it intraorally, and results from some type of trauma. The first patient I saw was an every 6 month-er. Never had any decay. Shows up one day with a small speck of brown in the center of #9. She had fallen in her home and hit her face on the floor and caused her nose to bleed an couple of months before. Did not report any dental trauma from the fall. I told her it was just a small pit decay and we’d fill it. She insisted on being anesthetized. So, I touched it with a drill and it started gushing blood. I called an endodontist friend and sent her straight to him. He did a root canal, reflected the gingiva to reveal the whole lesion, and place MTA and glass ionomer to restore. The third is a similar case, but on a young man. The second was in #31 due to severe bruxism or a couple punches to the jaw (he couldn’t swear to either). The first failed. The third is still working and the #31 was extracted because he couldn’t afford the treatment necessary. There may still be hope for your son’s #9. I can get you in touch with my endodontist friend who has done several cases with Advanced Cervical Resorption if you’d like, just shoot me an e-mail or call me.
One of my family members had #9 fracture off at the bone level. It had a root canal over 20 years ago and had a PFM on it since. He is severe dental phobic and comes only in an emergency. Calls me and tells me he broke his tooth. Sends me a text photo of it. I meet him at the office and start figuring out what I am going to do to get him temporized with a tooth. I did basically the same thing you did. I prepared a post space in both the anatomical crown and in the residual root structure. When I matched the upper and lower with a 3M fiber post in place, seated the post in the root structure. Then seated the “crown” on top of the post with 3M Rely X Universal. It was meant to last until we could add the tooth to his existing RPD. He has, of course, put that off several times because he is busy running his small business. Every time I see him or talk to him, in my mind, I hear, “Tick tock Tick Tock!” I know, like you do, that it is not a permanent solution. However, it is some pretty good “redneck engineering!” At least that’s what we call it up here in Tennessee! Good work. Nice photo documentation.
Thanks, Chad. I might want to chat with your endodontist friend. I was thinking of doing endo, laying a flap and restoring with Geristore (resin ionomer).
Well done Mike! You deserve a post Doc certificate in improvisation from the ANGUS MACGUYVER SCHOOL OF DENTISTRY!
For Your Consideration: Ortho-eruption, (and maybe perio-crown-lengthening), of the remaining #8 root so that you can get reasonable margins for a permanent crown?
And for the time being, somehow splint #8, (e.g with resin-saturated Ribond-fiberglass), to the her neighbours for extra stability?
Sorry to hear about this! Great job BTW!!!
Hi Mike,
I have the perfect solution for your son.
I am a technician and deal with this type of issue routinely.
I can mill a PMMA wing retainer with pontic.
We do it for juvenile ortho patients that need future implants.
Surgeons LOVE it when they do ridge augmentations as it doesn’t put any pressure on tissue/bone.
We call it “The death of Flipper”
Strong, Aesthetic and he wont have to remove it to eat or function normally.
Its bonded onto lingual of adjact teeth ,usually 6-11 and will looks great even after 3-4 yrs.
If you would like to discuss further, please call me at 678-714-7020
Regards,
Brian
Definitely it was very tough situation for you. However you have handled it very well. The procedure you have followed to handle this dental case is very good. Thanks for sharing this way with us.
Saw your son here in Colorado, tissue looks good considering everything
Tough kid! Good job!!
I missed this comment! Thanks SO much for seeing him, Gary!
Great job on your son- impressive work!! I read this and felt I should share my story. My own son at age 7 broke about 85% of #9 off when another kid ran right into his face and hit him square in the mouth with a laser tag gun at a birthday party. This also happened on a Sunday for me as well and I brought him into my office and bonded it. Luckily it was not a pulp exposure, he still had a wide open apex and now 4 years later the tooth has remained asymptomatic. He just got ortho and the orthodontist is going to force erupt it more so I’ll have more tooth to do a crown on when he’s finally old enough. In the meantime I’ll re-do the bonding which surprisingly has held up well. I was devastated when he broke his tooth because like you said- I knew that he would be facing other issues and even possibly loose the tooth someday. I also got the comments that he’s lucky his mom is a dentist, etc. I didn’t feel so lucky at all. In fact I asked why him? My beautiful son’s tooth wasn’t even fully erupted into his mouth when it was broken off!! So far we are lucky and I am hopeful that all he will need is a crown when he’s done growing. However, I will never get over him breaking his tooth and having to fix it. I never thought I would have my own son in the chair in that situation. It was heartbreaking. I hope things go well for your son with his future implants. I’m sure it has not been easy for you or him.
Thanks for sharing your story!
What’s the latest on your son’s centrals?
Also have you tried a buccally retained non prep bridge all in fibre reinforced composite. Accept that it’s thicker but it’s easy and simply removed when he’s at the implant point. Wonderful for trauma patient
Hello! I’ve had to rework it all a few times over the years. One of the centrals finally broke off. I “de-coronated” the root to the bone level and let the tissue heal in. I’ve bonded in a denture tooth as a “bridge” for now. We’re limping it along as long as possible. 🙂